This booklet series has been developed by specialist psychologists and medical doctors working in CNWL’s Sexual Problems Assessment and Treatment Service (SPATS). The information and exercises described in this booklet are based on psychological and sex therapy techniques that have been shown to improve sexual difficulties.
This series has been written for people of all genders, sexualities, sexual orientations, cultures, backgrounds and relationship statuses. While the suggestions and exercises in each booklet are based on principles that are relevant for everyone, some sections contain information about the biological and physical changes that can happen in specific parts of sexual anatomy. Some content and diagrams may not be reflective of your anatomy, including people who are intersex, people who have had gender affirming surgery, or people who have experienced physical changes due to specific medical conditions and/or treatment required. In these instances, if further information is required we recommend you speak to your GP or a specialist in sexual medicine. All bodies are different and we invite you to use the booklets in the way they are most applicable to you.
For further information, visit our Resources page.
Other booklets available in this series:
- Vulval pain during sex
- Enhancing sexual desire and enjoyment
- Anal pleasure
- Getting and keeping erections
- Ejaculating sooner than you would like
- Ejaculating later than you would like
This booklet provides information to help you better understand difficulties with vaginal penetration and the steps that you can take to start to overcome them.
-
Understanding difficulties with vaginal penetration
Information about what can cause difficulties with penetration.
-
Understanding arousal
Information about what happens to your body during sexual arousal.
-
General suggestions
Information about what can help improve difficulties with penetration.
-
Communicating with partners
Suggestions for communicating with partners about sex and sexual difficulties.
-
Frequently asked questions
Answers to some common questions about difficulties with painful sex.
-
Further support
Pain during vaginal penetration or attempted vaginal penetration can feel stinging, throbbing, burning, dry or sore. It can be sharp, dull or intense and it can occur at the start, throughout or after receptive penetrative sex.
This booklet is aimed at people who experience pain or discomfort during, or when attempting, penetrative vaginal sex. Some people also experience pain when the outside of their genitals are touched. Please see our Enhancing sexual desire and enjoyment booklet if this applies to you.
The level of pain can range from mild to severe. Sometimes penetration can feel impossible, and repeated unsuccessful attempts can leave you feeling frightened and frustrated. It is understandable that having these kinds of experiences may result in wanting to avoid sex altogether.
For many people with a vagina, any penetration may be painful including using tampons during smear tests, medical examinations and during sex.
Pain during sex is fairly common and can occur for many different reasons, but it is not something you should endure and should always be checked out by a medical professional.
What can cause or contribute to difficulties with penetration?
There are a variety of reasons that you might experience difficulties with painful sex, and is often a combination of physical or medical factors along with psychological and/or relationship influences.
A number of physical or medical factors can cause and contribute to difficulties with penetrative pain. They include:
- Genital infections and imbalances such as thrush or bacterial vaginosis
- A sexually transmitted infection
- Dermatological (skin) problems (for example, lichen sclerosis or eczema)
- Gynaecological problems (for example, endometriosis or fibroids)
- Pelvic floor problems and dysfunction
- Hormonal changes or endocrine disorders (like diabetes)
- Changes associated with pregnancy, birth, or breast feeding
- Ageing or menopause-related changes
- Irritable bowel syndrome
It is important to have a thorough medical assessment by an appropriately trained medical professional, such as a specialist in sexual problems, to ascertain the role of any physical or medical factors contributing to penetration difficulties. Assessment of pain during penetration will usually involve an physical examination, This doesn’t have to happen at the first visit and your clinician will work with you to perform an examination in a way that you are comfortable with. It is important to note that, if you do not have an examination, then there is a chance that you are missing a treatable factor contributing to pain during sex, and therefore will be less likely to achieve your goal of reducing pain during penetration.
Difficulties with vaginal penetration can also be related to psychological factors including:
-
Beliefs about sex (for example, that it is shameful)
-
Not feeling safe with your partner
-
Unwanted, or negative, previous sexual experiences
-
Worrying about or expecting sex to be painful
-
Not being aroused by the situation, feeling sexually bored, or other feelings about your sexual practices and partners
-
Stress, depression, and anxiety
-
Tiredness
-
Relationship problems
-
Body image concerns
-
Having other things on your mind and not being able to be in the sexual moment
-
Having another sexual difficulty, or your partner experiencing sexual difficulties
Some people might never find out what has caused their difficulties with penetration, and there might be a number of factors involved in causing and maintaining the problem.
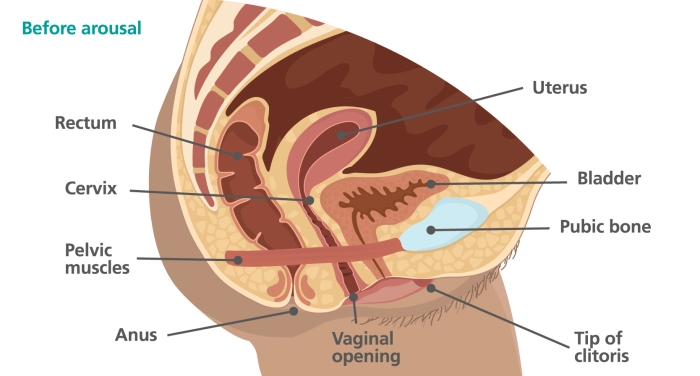
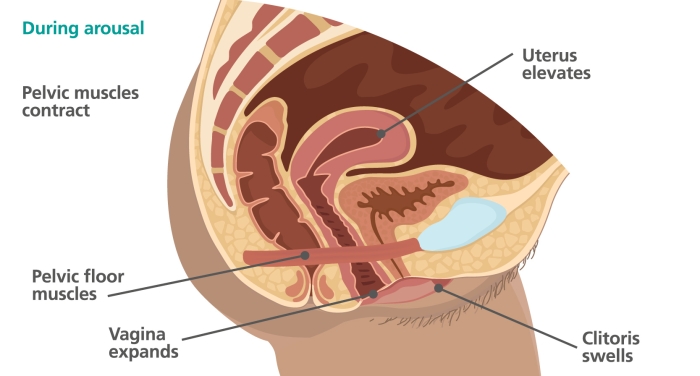
When you are aroused, chemical messages and hormones are sent around your body which allow physical changes to take place such as:
-
your heart rate and blood pressure increase
-
blood flows to your genitals
-
Some of your muscles tense
-
your heart beats faster
-
your breathing becomes faster and deeper
Increased blood flow means your clitoris becomes bigger and more sensitive to touch, although you still might not be able to see it under its hood. Your labia swell, and you might notice that you start to get wet as your vaginal walls produce lubrication. The vagina expands in size and the uterus lifts up, which lengthens the vagina.
The image below shows some of these physical changes:
These physical changes prepare your body for sexual contact, and can make touch feel more comfortable and enjoyable. It is important that you give your body time to respond during the arousal process so that you don’t feel any discomfort during a sexual experience. It is also important that you feel confident talking about this with your sexual partners so they can understand and respond to your feedback about how turned on you feel. If anything gets in the way of the arousal process, then these physical changes may not happen and your body won't be prepared for sex. This can cause penetration to be uncomfortable or painful.
The impact of anxiety on arousal
The arousal process is controlled by a part of the nervous system called the parasympathetic nervous system (PNS), which is an involuntary, or automatic, system that is active when our mind and body is in ‘calm’ mode.
There is another system in the body, called the sympathetic nervous system (SNS), which works in opposition to the PNS - when one is in control, the other closes down. The SNS controls the brain and body when we feel stressed, anxious, or in danger (in ‘stress’ mode). This is sometimes called the ‘fight or flight response’. When the flight or fight response is activated, it sends blood to the muscles we need to run or fight (for example, our arms and legs) and shuts down all non-essential functions that we wouldn’t need if we were in danger, including the arousal system.
The diagram below demonstrates the impact these two systems have on the body (see the bottom of the page for a text description):
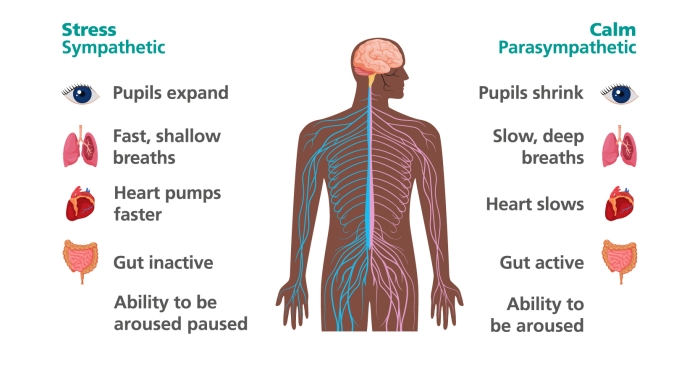
The fight or flight response can kick in for both real or perceived/imagined threats, meaning that worrying about something is enough to trigger these physical changes in our bodies. As shown in the diagrams, the body has to be relaxed (or in ‘calm’ mode) in order to become sexually aroused. When you’re anxious or worried (whether about being in a sexual situation or about anything else), your body switches into ‘stress’ mode) which pauses the arousal system.
This means that there may be less lubrication, the vagina may not relax or lengthen, and the uterus may not tilt to allow more room inside. Any or all of these things can contribute to difficulties with penetration.
The image is a medical diagram - the impact of the ‘Stress’ or Sympathetic Nervous System and the ‘Calm’ or Parasympathetic Nervous System on the body.
The labels for the 'Stress' system include:
- pupils expand
- fast, shallow breaths
- heart pumps faster
- gut inactive
- and ability to be aroused is paused
The labels for the 'Calm' system include:
- pupils shrink
- slow, deep breaths
- heart slows
- gut active
- and ability to be aroused
To improve difficulties with penetration, it is important to:
- Have sex only when you want to
- Feel safe in your sexual relations
- Understand and Meet your own conditions for good sex (for example having privacy, feeling relaxed, not feeling rushed, pressured, tired or distracted, feeling able to trust a partner)
- Learn to recognise when you are tense and identify techniques and ways to relax and overcome this
- Use self-exploration to identify the kind of stimulation you like and focus on this stimulation during partnered sexual activity
- Be able to enjoy having sex rather than worrying about your performance or what you look like
- Feel confident to communicate and negotiate about sex with your sexual partners
When pain is felt only on deep penetration, it is important to exclude a medical cause for the pain by having an assessment with a medical doctor. Once you have excluded a medical cause for the pain, it may be helpful to avoid certain positions, for example being penetrated from behind (when penetration may be deeper and may involve contact with the cervix). If you suspect this is the cause of pain for you, you may wish to try the following positions to see if they are more comfortable:
- being on top, where you can control the depth of penetration;
- being on your back and raising your legs high;
- or being on your back with your legs together (usually you’ll need to have your legs apart for your partner to enter, then put your legs together, with your partner’s legs on the outside of yours).
The vagina’s production of natural lubricant can be affected by a range of factors (for example: pregnancy, breastfeeding, the menopausal transition and certain medications). If your vagina feels dry, you can try to make sex more comfortable by getting more turned on before penetrative sex and/or by using a lubricant (lube), which you can buy at any chemist or sex shop. Lots of people find that lube makes intimate touching more pleasurable.
Lifestyle factors
A healthy lifestyle helps to reduce stress levels and improve cardiovascular health. In turn, this can enhance arousal and support sexual functioning. A healthy lifestyle can be supported by:
- Getting enough sleep
- Eating well
- Exercising regularly
- Stopping smoking
- Limiting the use of alcohol and recreational drugs
Visit nhs.uk/live-well for help and advice around maintaining a healthy lifestyle.
We know that there are three key elements that enable sex to go as well as possible: psychological arousal, physical touch, and being in the moment. These are known as the Conditions for Good Sex (Gurney, 2020).
Psychological arousal refers to how much of what is happening you find sexually arousing and turns you on. This can include how attracted you feel to your sexual partner(s), things in the environment (like lighting, sounds), the context (time of day, your role in the sexual experience), and also sexual fantasy and types of porn.
Physical touch refers to the types of physical stimulation that your body needs to feel sexually aroused. This can include the types of pressures your body needs, the speed and location of touch, the types of sex you enjoy and whether you enjoy using sex toys and/or lubricant (‘lube’).
Being in the moment refers to how much you are able to be in the present moment (rather than caught up in other thoughts or worries) and how much you’re able to focus on the physical sensations and psychologically arousing stimulation. This also includes how much you’re able to feel relaxed. Later in this booklet we have included suggestions about using mindfulness to increase being in the present moment.
The closer each of these elements are to our ideal conditions, the better the sexual experience will be. If we have high psychological arousal (are aroused and turned on), are receiving the types of physical touch we find pleasurable and are able to be in the present moment (and not distracted by other thoughts or worries) we have met the conditions we need in order for sex to go well.
Knowing your own conditions for good sex can help you to:
- understand what you need for sex to be its most enjoyable
- understand what might be disrupting the arousal process
- understand how these conditions might have changed or been impacted by sexual difficulties
It is not usually necessary for all of your conditions for good sex to be met throughout every sexual experience for the experience to be enjoyable. However, understanding your own conditions, and talking about them with sexual partners, can help to include more of your conditions more of the time.
Our pelvic floor muscles are like ‘a bowl of muscle’ underneath the pelvis. They provide support for the pelvic organs and help control when we go to the toilet. They also help to increase blood flow to your genitals which aids arousal and increases pleasure. Contractions of these muscles also help produce sensations at orgasm.
The image below shows where your pelvic floor muscles are on your body. You can feel your pelvic floor muscles by contracting your anus as though you’re trying to stop a bowel movement, then imagine a zip closing forwards an upwards as if you’re trying to stop the flow of urine at the same time.
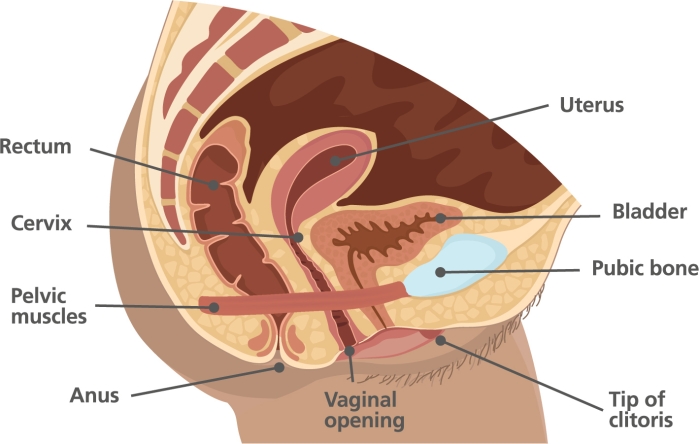
Sometimes, the muscles of the pelvic floor can become tight or tense. There are many reasons why this happens, for example injury during surgery or childbirth, a history of sexual trauma, feeling anxious about sex for any reason, or just the anticipation of penetration. This tension can cause pain or discomfort during sexual activity, and reduce pleasure.
Pelvic floor relaxation exercises improve your awareness of when these muscles are tense or relaxed. Ensuring our pelvic floor muscles are relaxed helps sex to be enjoyable and not uncomfortable or painful.
To practise pelvic floor relaxation, you can use a technique called ‘Sniff, Flop and Drop’.
- Sniff - take a soft and deep breath in through the nose over three seconds. Keep your shoulders relaxed and your chest still.
- Flop - keep your stomach soft while breathing in. This should mean that the abdomen ‘flops’ or fills all the way out on the in-breath.
- Drop – allow your pelvic floor to drop or release also during the in-breath.
You might find it easier to close your eyes while doing the exercises to really focus on the sensation of the pelvic floor relaxing, of ‘dropping away’. You can then take this skill into sexual situations, consciously relaxing your muscles in the sexual moment.
Earlier in this booklet we explained the importance of being in the present moment to fully enjoy sex. ‘Mindfulness’ has its roots within a wider set of Buddhist spiritual teachings and practices, the benefits of which have been known to Asian communities for centuries. More recently, a secular version of mindfulness practice has been adopted by Western cultures. Mindfulness practice can enhance our connection to the present moment, which can help improve a range of difficulties, including sexual ones.
When we get caught up with critical thoughts or trying to change things, this takes us away from the present. An important part of mindfulness is paying attention to your present experience without evaluating it. This means not judging the experience that you are having, just noticing it with curiosity and openness.
There are many ways to practise mindfulness. For example you could:
- Go on a walk and use all your senses to notice your present moment experience – the different things (like colours and textures) you can see, the smells and the sounds. Rather than ‘listing’ the things you notice, this is about really experiencing them in depth and detail.
- Sit in comfortable position, with your feet on the floor and your back straight but relaxed. Spend some time focusing on your breath as you inhale and exhale, focusing your awareness on the natural rhythm of your breathing.
It is completely normal for your mind to wander. When you notice this has happened, gently bring the focus of your attention back to the present moment.
It can take time to increase your ability to be mindful. You can start by practising for 10 minutes each day as you get more confident. Building up your day to day mindfulness skills can help you stay more present during sexual situations. Everyone responds differently to mindfulness practice, however. As with all suggestions in this booklet, only do what feels right for you and stop if anything causes you pain or feels distressing.
We are all unique when it comes to sex. Our partners cannot read our minds. They are very likely to have had different experiences of sex, and be holding different assumptions, beliefs and preferences to our own.
Good communication can help you to:
- Get closer to the sex life you want by sharing your conditions for good sex
- Meet your partners’ needs by better understanding their conditions for good sex
- Allow your partners to understand any sexual problems you might be having and what they can do to help
- Build trust and intimacy in your relationships
What gets in the way of communicating about sex?
- Not realising or believing it’s important e.g. “good sex should just happen naturally”
- Feeling awkward or embarrassed
- Fear of rejection
- Worrying it will spoil the moment
- Feeling unsure what you want to say or how to say it
Take some time to think about your intentions in advance
What is it that you would like your partner to know? If the conversation went well, what would be different at the end of it? Planning ahead can helps to reduce your own anxiety and increase the chance of your partner being able to understand what you want them to hear.
Think about timing
Avoid having any difficult conversations about sex in bed, or just before/ after sex. You might want to plan the conversation for a later date to avoid putting your partner(s) on the spot. Choose a time when you won’t feel rushed, and have plenty of privacy. Avoid talking about sex or sexual problems during an argument, when you have been drinking or using drugs or when you are tired or stressed.
Put yourself in your partner’s shoes
Remember that they might feel vulnerable or embarrassed. How might it feel for them to hear what you have to say? Offering plenty of reassurance and appreciation can help them to feel comfortable.
Have a two-way conversation
Encourage your partner to share their own thoughts, feelings and preferences with you. Listen carefully to what they have to say without interrupting. Let them know you can understand their perspective (even if you might feel differently about some things). Thank them for being open and honest with you.
Use ‘I’ statements
Using sentences that start with ‘I’ rather than ‘you’ help ensure that we are communicating clearly from our own perspective. It also reduces the risk of the other person feeling judged or blamed. For example, say “I’d like us to try having sex differently” rather than “You always want to have sex the same way” or “You need to change”.
Approach the conversation with positivity and with solutions in mind
Frame the conversation as an exciting opportunity to try new things and expand your sexual relationship together. It can be helpful to be ready with some suggestions or requests to share with your partner to help move things forward. Focus more on talking about what you like, want more of or want to try rather than what you don’t like or want.
Keep the conversation going
Getting into the habit of regularly checking in about sex can help to reduce any awkwardness and anxiety we might feel. It can also make it easier to bring up any difficulties or problems with sex that you and your partner(s) might have in the future.
Is it normal to experience pain the first time you have penetrative sex?
It is fairly common to experience some pain or discomfort the first time you have penetrative sex. If you grew up hearing stories about sex being painful this can sometimes lead to painful experiences of sex — because when we are expecting pain we are less likely to get turned on. Feeling worried or anxious about any aspect of penetrative sex or attempting penetration before being turned on enough can also lead to some pain or discomfort.
Should I try and ‘push through the pain’?
It is important not to continue having penetrative sex that is painful. Many people feel under pressure from their partner or themselves to ‘push through the pain’. This can increase the association your body has with sex being painful, and lead to more anxiety around sex. Focus instead on types of sexual touch that are not painful and give you pleasure while you seek support to overcome the difficulties with penetration.
How can I practise safer sex?
There are a number of ways in which you can have safer sex in order to protect yourself and partners from sexually transmitted infections (STIs) and from unwanted pregnancy. These include using condoms, pre-exposure prophylaxis (PrEP), to protect against the transmission of HIV, and different contraceptive methods.
In this booklet, we have chosen not to refer to any one of these specific methods, and encourage you to make your own decisions about protecting yourself and others in each instance of sexual activity you undertake. Your local sexual health clinic can provide you with free STI testing and information and advice on practising safer sex.
Additional STL resources
Sex Therapy London is a website developed by clinical psychologists at Central and North West London (CNWL) NHS Foundation Trust who specialise in sexual health and sexual difficulties. This website contains a range of self-help information, advice and resources to help improve your sex life. It also has free interactive online programmes for people experiencing sexual difficulties that are available to patients of CNWL Sexual Health Services.
Further support
Within the United Kingdom, if you need further information, support or advice about your sexual difficulties there are a number of options available to you.
Sexual difficulties can sometimes be connected to an underlying health problem, so making an appointment to discuss this with your GP is an important step. Your doctor may also be able to refer you on for any specialist support you might need.
Psychosexual therapy is sometimes available via the NHS. Your GP or your local sexual health clinic can help you access this in your local area.
You can also access psychosexual therapy via the Relate website or by finding a private, specially trained psychosexual therapist on the Cosrt website. Other private therapy providers are available.